Sleep Disordered Breathing: A must read for Parents
A growing area of healthcare involving awareness of the upper airway and its relationship towards Sleep Disordered Breathing (SDB) has resulted in a paradigm shift in dentistry towards the need for early identification of signs/symptoms of SDB to prevent the multitude of health complications that accompany its occurrence. Even more crucial is that parents and patients alike understand early in their child’s development the importance of a correctly functioning nasal oral complex and how to address the causes of SDB and crooked teeth instead of treating the symptoms later in life. 80-90% of craniofacial growth occurs between birth and age 12 (24). There are early preventative, less invasive treatment options for children that allow for more natural development and stable results, but with this comes the need for awareness.
SDB includes a spectrum of disorders including but not limited to snoring/loud breathing, air-flow limitation problems (UARS), hypoventilation, and the most well-known sleep apnea. SDB is much more critical and underdiagnosed than has been previously thought and has now been reported as an epidemic. It can be easily overlooked and often is left untreated. Over 20 years of research has identified an association between SDB and crowded or crooked teeth and other dental concerns. SDB can have a lasting impact on your child’s growth and development and even impact learning and create behavior challenges similar to ADD/ADHD. A 2013 Meta-analysis suggested a medium correlation between ADHD and SDB (26), and recent research has demonstrated 75% of children with ADHD also have a sleep disorder (6).In addition, SDB has been increasingly linked to lower IQs, trouble learning, emotional problems, and nighttime disturbances such as sleep walking, parasomnias, and bedwetting (4,6,7,8,9,10,18,20,25,26,29). In a 2012 study of 11,000 children, early-life SDB symptoms had, “strong, persistent statistical effects on subsequent behavior in children.” The findings suggest that SDB symptoms may require attention as early as the first year of life (3).
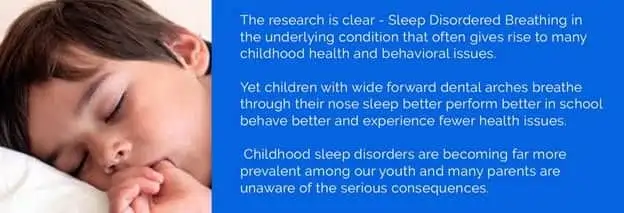
Many health professionals believe that a child does not grow out of SDB but grows into it, and the signs and symptoms change over time with the potential “end stage” being sleep apnea and the co-morbidities that follow. In other words, pediatric sleep disordered breathing may put a child at a higher risk for worsened SDB in the future (16). It is a misconception to think just because a child “sleeps” fine they may not have the potential for sleep disordered breathing. The central issue in children and adults with SDB is a compromised airway.
In children, developmental and functional abnormalities can have a lasting impact on overall development, specifically craniofacial growth (naso-maxillary complex and mandible) and ultimately the size of the upper airway. This, in association with sleep, is what leads to SDB. Overall, craniofacial growth is influenced by genetic mutations, environmental factors and both environmental factors acting with genes (epigenetics) (13). We all want straight teeth, but what most fail to realize is our smiles are also a reflection of our oral function, and by failing to establish a healthy oral nasal complex, we are not only setting ourselves up for orthodontic failure (hence the need for retainers), but we are ignoring the underlying issues that can impact a lifetime of health and development. What is most important to note is that the signs and symptoms of SDB can be identified very early in a child’s development and treated before they evolve into chronic airway management problems, (like apnea) facial malformation, or malocclusion. Even children without SDB will benefit from early intervention and treatment of oral habits and abnormalities that have the potential to influence facial development, and with this they can improve their quality of life and prevent airway management issues in their future. It is important you talk with your dentist and or family physician if you notice your child is displaying signs of SDB.
Signs and Symptoms of SDB may include (2,21,31,30):
Snoring * The American Academy of Pediatrics recommends that all children/adolescents be screened for snoring and that all children/adolescents who snore and have symptoms of OSA require a sleep study.*
- Non-infected swollen tonsils and adenoids
- Frequent ear and upper respiratory infections
- Daytime fatigue (Presents as hyperactivity in some children)
- ADHD/ ADD behavior and or diagnosis
- Behavior and socialization issues (depression, irritability, mood instability)
- Nasal obstruction/resistance (congestion) and Rhinitis
- Headaches (morning)
- Venous Pooling under eyes (Allergic Shiners)
- Learning and Cognitive issues/Decreased IQ
- Poor memory and ability to focus
- Digestive issues- GERD/LPR
- Frequent nighttime awakenings/ Night Terrors/restless sleep
- Bed Wetting
- Drooling Day or Night (sign of mouth breathing)
- Autonomic imbalance
- Blood pressure and cardiac issues
- Sleep parasomnias
- Sleep walking
- Diaphoresis (Night sweating)
- Failure to Thrive
- Witness apneas
- Gasping or loud breathing
- Mouth breathing
Your dentist or doctor may notice other physical signs of SDB and improper facial development factors including but not limited to (2,21,31,30):
- Teeth grinding (bruxism)or clenching
- Long face syndrome
- Mouth breathing/Open Mouth Posture
- Midface deficiency
- High vaulted palate
- Oropharynx crowding
- A narrow upper jaw or palate
- Micrognathia (small jaws)
- A noticeable underbite or overbite
- Crowding of teeth
- Hypermobility/laxity of tissues
- Improper tongue positioning
- Tongue tie
- Nasal atropy/inflammation
- Speech Problems-hyponasal
- Deviated nasal septum
- Dry Lips
- Bulging nasal turbinate
- Allergies
- Lingually inclined teeth
- Tongue thrusts
- Improper swallowing
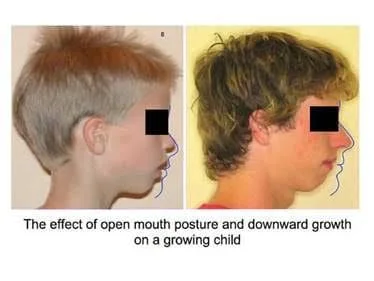
One often unexplored mode of breathing that impacts facial development and SDB is mouth breathing. Most parents have no idea that mouth breathing could stunt or limit their child’s mental status or development. It is actually nasal breathing is the most natural and beneficial way to breathe and distribute oxygen to our tissues. Children with orthodontic abnormalities are 4 times more likely to be chronic mouth breathers. Prolonged mouth breathing can cause dental malformation including increased face height (long face syndrome), retrognathic (regressed) jaw position, low tongue posture (poor arch development), gummy smiles and multiple unattractive abnormal growth patterns of the face(24).

One reason nasal breathing is essential is because it is responsible for the production of nitric oxide in the nose. Nitric oxide is a vasodilator and is responsible for increasing oxygen transport throughout the body. It is crucial for smooth muscle operation and overall health. By mouth breathing, you not only decrease oxygen to your brain and body, you interrupt sleep patterns. Mouth breathers have a lower amount of oxygen in their blood as compared to nasal breathers -18% more when nasal breathing (14). Diaphragmatic and nasal breathing is most important to best circulate and produce nitric oxide in the body. This knowledge has even led to new training strategies involving nasal breathing for elite athletes for enhanced performance, yet nothing is more importance than its role in development of a child.
Hypertrophied tonsils and adenoids can occur due to a variety of reasons and can impact SDB because they, along with other inflammatory factors, can lead to impaired nasal breathing. When we mouth breathe our first line of defenses against pathogens is eliminated. This often leaves mouth breathers with respiratory infections, and narrow nostrils, allergic rhinitis, asthma, adenoids and tonsil hypertrophy (enlargement), a deviated septum, and open postured lips (1). Mouth breathing also leads to bad breath, dry mouth, and periodontal disease (inflamed oral tissues) (29). Dry mouth reduces saliva which has preventative role in cavity and tooth decay. Therefore, mouth breathing too may increase potential for cavities.
Hypertrophied tonsils

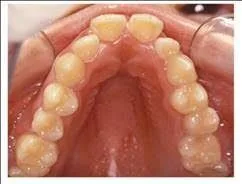
High vaulted narrow arc
Mouth breathing also leads to functional changes, including abnormal swallowing, feeding, and occurrence of esophageal reflux (13). It is also is important to note that form follows function yet function follows form. Already present craniofacial abnormalities along with nasal obstruction, obesity, or hypertrophied tissues can prevent nasal breathing and can make SDB symptoms progressively worse. It is important to recognize the need for fellow health care professionals such as your family physician, ENTs, sleep, speech therapists, and myofunctional therapists to help identify what factors are contributing to airway restriction/obstruction. The first step towards solving any airway SDB issue is the restoration of nasal breathing.
Another important overlooked, yet preventable, factor that can also be caused with or without mouth breathing is low tongue posture and tongue thrust/reverse swallow. There is a strong relationship between chronic mouth breathing, open bite occlusion, and tongue thrusting (replacing ant teeth).The tongue has a primary role in protecting the airway and is a driver for development of the face. In order to best obtain normal facial development, a child must have normal resting tongue posture at the top of the mouth. Without the tongue to expand the anterior and lateral arches of the palate, the palate becomes vaulted and the teeth become crowded. This further exasperates SDB as the airway space too is compromised by the tongue especially during sleep as the potential increases for it to fall into airway space during sleep.
If a child has a tongue tied or lip tied (tight maxillary and lingual frenulum attachments), he or she will not be able to rest the tongue on top of the palate nor gather food at the top of the mouth for a proper swallow. More recent research in the area of sleep medicine has even demonstrated the presence of an untreated tongue tie at birth is associated with an increased likelihood of Obstructive Sleep Apnea in the future (15). In addition to its relationship to sleep disordered breathing, tongue ties are associated with speech articulation issues, reflux, indigestion, GERD, dental problems, headaches, and TMJ disorder. It is important that tongue function is evaluated soon after birth in order to have the best breastfeeding outcomes and best stimulate the musculature and positioning which favors the development of nasal breathing.
4-10%of newborns are believed to be born with tongue ties
39,482 babies are born in Iowa each year
1,579 - 3,942
babies in the state of Iowa are affected by a tongue tie each year
Oral habits such as thumb sucking, bottle feeding, and pacifier use also have a strong potential for negatively influencing oral musculature of the mouth and have been strongly associated with malocclusion, an increased rate of ear infection, abnormal swallowing and tongue position, and mouth breathing (5,11,23). Children with deep dental bites are 2.8x more likely to have ear tubes placed or recommended by a pediatric otolaryngologist (3). In addition, pacifier use is associated with an even higher risk of developing more malocclusion than digit sucking and appear to be a preventable and significant risk factor for ear infection prevention (5,2).Infants that are bottle fed exhibit different nutritive sucking patterns and are less likely to become nasal breathers. Early weaning from breastfeeding can have the same effect and result in open mouth posturing and mouth breathing (1).Children who are bottle fed and those who have prolonged pacifier use should be screened early on for the effects of mouth breathing, tongue thrusting, high palatal arch formation and abnormal mechanics during swallowing.
Open bite from pacifier user

Diagnosis and treatment of airway obstruction, incorrect mode of breathing, malocclusion and identification of other underlying causes is crucial to allow earlier orthopedic treatment which can be more effective, natural, less restrictive, and more stable over a life time. Most importantly, it can allow for natural form and function by treating the causes of these issues not just treating the symptoms that can occur later in life such as TMD/TMJ disorders, insomnia, UARS, and sleep apnea.
Routine early examination can screen for craniofacial deformities and is important to ensure the infant is developing good oral habits. At birth proper screening of Tethered Oral Tissues (TOTs) should be performed and resolved if identified. By age 2-3 dental signs of nasal obstruction, malocclusion and mouth breathing can be identified and treated. Through education, early orthodontic intervention, (such as Myobrace, Healthy Start or palatal expansion) myofunctional therapy and possible evaluation by other specialties, we can help your child eliminate damaging habits, improve oxygenation through correct breathing, all while improving behavior, sleep, learning, and sports performance. Most importantly this may allow for your child to reach their full potential. Beautiful Straight Teeth are the icing on the cake, the desired result of a properly functioning oral nasal complex.

If you have concerns your child may be experiencing sleep disordered breathing or would like to learn more about how to prevent airway issues, please contact Rock Valley Dental today. Dr. Koth and his staff are proud to be a part of airway focused dentistry and are very passionate about helping children achieve a lifetime of oral and airway health.